
Here, she tells us how she came to work in respiratory care and the way she has strived to make a difference in nursing.

“As a child, I always wanted to be a nurse, I’ve no idea why. There’s a photograph of myself age approximately five, in a nurse play uniform.”
Linda’s automatic response on why she chose to be a nurse tells us she was always going to be one. She started training at Orsett Hospital, which was part of Basildon & Thurrock Hospitals, at 17 years old, qualifying in 1977. Her first stint was on a surgical ward, and she’d also applied to undertake midwifery training.
“I qualified as a Midwife in 1979. Because I was already a State Registered Nurse, the course was shortened, so it took two years rather than three,” she tells us. Linda loved her role as a Midwife, and it all seemed very fitting as she soon became pregnant with her first child. “I was keen to go back to midwifery but the only way I was allowed to go back was if I fitted in with their shifts,” she explains. Linda says this was a time when mothers didn’t leave their children with a childminder.
Putting family first, Linda decided to move away from midwifery. Starting a role as a District Nurse was perfect. “They were advertising for district nurses to work twilight service. Working three or four evenings sort of satisfied me. It was working with people who needed all the usual district nurse-type care,” she says.
A couple of years later and Linda found herself moving to Felixstowe. “I got asked to help out at the Port of Felixstowe in the occupational health department. I started doing a few hours and I got offered a permanent post,” she tells us.
“There were only two practices in Felixstowe. I did some holiday cover at both practices. I realised I liked developing things, without me necessarily being aware, as I had in the Occupational Health Nurse role, and the move from occupational health to practice nursing was sealed!”
Linda gained her certificate in Occupational Health Nursing, and this is where she was first curious about respiratory care. Linda was working on cases of occupational induced asthma which evoked her interest in respiratory disease. This was also a time when practice nursing was evolving, she reminds us.
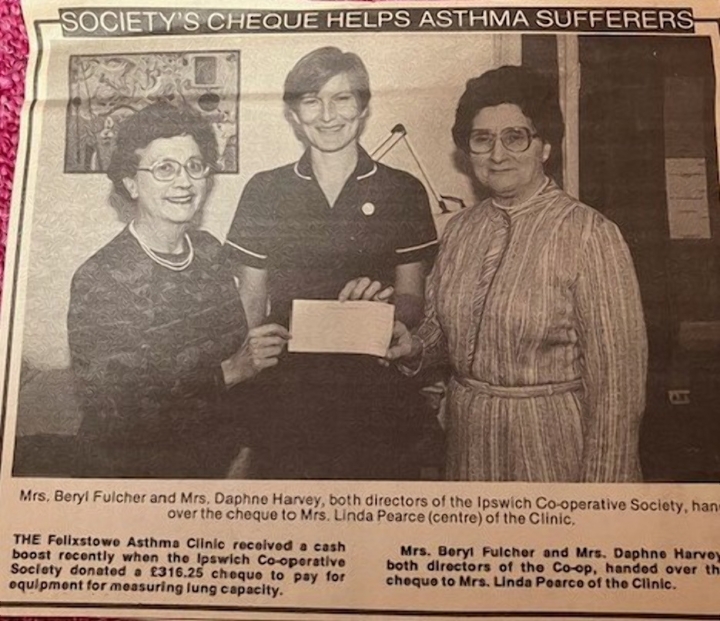
If there’s one thing Linda is proudest of in her nursing career, it’s the nurse-led asthma clinic she set up. She had practice nurses asking to sit in on the clinics. The training helped them to complete their asthma diplomas. For her, sitting with the practice nurses and helping them establish in their own way was important, and is something she’s still proud of today.
“I took over the asthma management within the practice. This was when asthma training was developing. I set up a Suffolk asthma course for practice nurses. It wasn’t validated like it would have to be now, but it was very much about asthma management.”
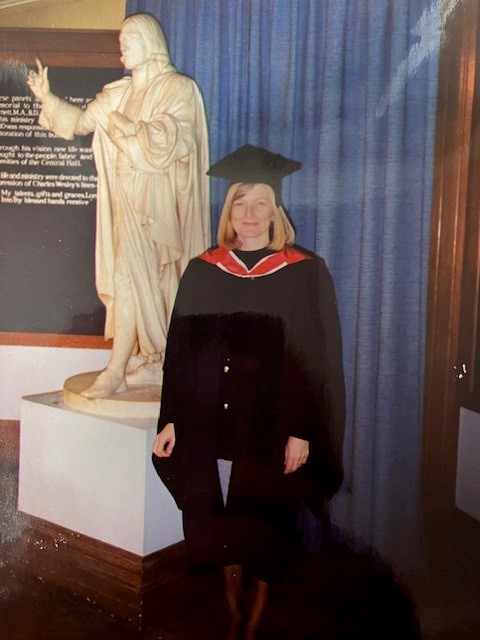
During the early 1990’s the Nurse Practitioner diploma was rolled out at the Royal College of Nursing (RCN). It’s a qualification that Linda took on while working in the practice. She also completed a Master’s degree in Life Sciences at University of East Anglia. “I was the second cohort in the Nurse Practitioner diploma. And that was one day a week going up to the RCN. I think I was a bit of a workaholic really!”

In the late 1990s, Linda was introduced to a Respiratory Consultant at West Suffolk Hospital. The introduction was the start of Linda’s influence at West Suffolk Hospital.
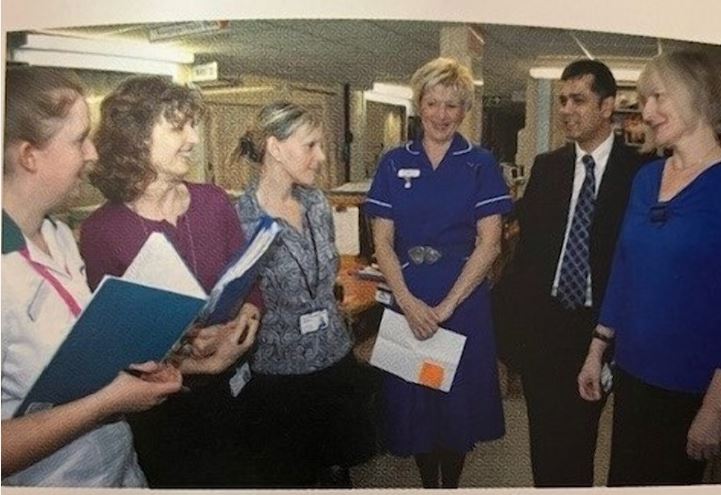
“I joined as a Specialist Nurse. I thoroughly enjoyed it and I had quite a lot of autonomy. I saw patients on the wards, in outpatients and I supported a lot of the nurses in completing their asthma diplomas.”
Picture courtesy of West Suffolk NHS Foundation Trust
One key theme Linda highlighted was the support and mentorship she had from General Practitioners (GPs) and Medical Consultants throughout her career. “It was the doctors who supported me. There was one in the early days for setting up the asthma clinic. There was another GP when I wanted to develop my role further as a nurse practitioner, and the one in the hospital, as well,” she tells us.
“I was appointed Nurse Consultant after going through a rigorous interview. As an internal candidate, that was incredibly daunting, because everybody knows your weaknesses. But I did it, I got the post.”
Linda explains as a Specialist Nurse, you’re at the ‘top of the tree’ in terms of your next move. In 2001, the Nurse Consultant post was created, and this was an exciting prospect for those in specialist nursing roles.
Linda always strived to make a difference in nursing. While she could have left nursing and trained to be a medical doctor, she wanted to show what could be achieved with nursing. “As a Consultant, it was conditional for me to complete a doctorate in nursing. I completed this in 2008, with my thesis focusing on non-drug management of breathlessness in COPD.”

Linda has sat on various advisory boards and committees throughout her career and was a Visiting Fellow at Essex University. She held the Suffolk representative role on the East of England respiratory board, was West Anglia Clinical Local Respiratory Network Lead, and was a member of BTS/SIGN asthma pharmacology management review group.
Linda was also one of the reviewers during the National Review of Asthma Deaths (NRAD), became the Clinical Lead for the Suffolk COPD services and was a member of the National Strategic Clinical Network for paediatric asthma in the East of England. “In general practice, I saw all age groups in the asthma clinic. When I started working at West Suffolk Hospital, I felt there was a lack of transition from paediatric asthma to adult asthma. So, I got involved in setting up a transition clinic, which then morphed into a once-a-month paediatric asthma clinic.”

The efforts of Linda and her team weren’t overlooked, winning an array of accolades between 2010 and 2015.
“We were a winner of the NHS Innovation, winner of the General Practice Nurse Clinical Team of the Year for Respiratory Care, and we got the British Thoracic Society Integration of Respiratory Services award. That was special, for setting up the COPD service across primary and secondary care.”
Linda tells us she broke a lot of barriers during her nursing career. “I never thought of myself as ambitious. I think I had to be driven to be able to get through the barriers.” Linda believes doing this has created more opportunities for aspiring nurses. Looking back to her training days, she recalls one experience with a colleague. “I always remember a colleague coming from one of the London hospitals and the nurses weren’t even allowed to take blood pressure readings. The doctors took it. That’s how archaic it was. It’s great looking at where nursing is now.”
Retiring from clinical practice in 2022, Linda had intended to continue clinic work in primary care. However, expectations proved a little too much.
“What I’m doing now is the teaching side of things, which I absolutely love. And I’m continuing to write articles. That keeps me up to date as well.”
Her diverse roles over the years and direct contact with patients from different walks of life have helped Linda approach patient care effectively. “One of my strengths was understanding the world that people live in. My roles helped strengthen my understanding when working in respiratory medicine. It’s looking at the broader picture, understanding how you can support people in the context of their lifestyle.” Linda says this is much like telling patients to stop smoking. “It’s a good health message, but it needs to be done in the context of their lifestyle, as well.”
Words of wisdom
If Linda had one piece of advice for anyone starting out in respiratory nursing, it would be to have confidence in your own abilities. “Try and have a bit of a structure as to what you want to achieve and know that you can get there. If I can achieve it, anybody can.”





